Are Benign Tumors Are Likely to Spread to Different Parts of the Family?
| Benign tumor | |
|---|---|
| Other names | non-cancerous tumor |
 | |
| Normal epidermis and dermis with intradermal nevus, 10x-cropped | |
| Specialty | Oncology, Pathology |
A benign tumor is a mass of cells (tumor) that lacks the ability either to invade neighboring tissue or metastasize (spread throughout the body). When removed, benign tumors usually practice not grow back, whereas cancerous tumors are malignant and sometimes exercise. Unlike about benign tumors elsewhere in the body, beneficial brain tumors tin be life-threatening.[ane] Beneficial tumors generally have a slower growth rate than cancerous tumors and the tumor cells are ordinarily more differentiated (cells accept more normal features).[2] [3] [iv] They are typically surrounded past an outer surface (gristly sheath of connective tissue) or stay contained within the epithelium.[5] Mutual examples of beneficial tumors include moles and uterine fibroids.
Although benign tumors volition non metastasize or locally invade tissues, some types may still produce negative health effects. The growth of benign tumors produces a "mass effect" that tin compress tissues and may cause nerve impairment, reduction of claret catamenia to an surface area of the torso (ischaemia), tissue decease (necrosis) and organ damage. The wellness effects of the tumor may be more prominent if the tumor is inside an enclosed space such as the cranium, respiratory tract, sinus or inside bones. Tumors of endocrine tissues may overproduce certain hormones. Examples include thyroid adenomas and adrenocortical adenomas.[2]
Although well-nigh benign tumors are not life-threatening, many types of benign tumors take the potential to get cancerous (malignant) through a process known as tumor progression.[vi] For this reason and other possible negative health effects, some benign tumors are removed by surgery.[7]
Signs and symptoms [edit]
Benign tumors are very diverse; they may be asymptomatic or may cause specific symptoms, depending on their anatomic location and tissue type. They grow outward, producing large, rounded masses which can cause what is known as a "mass effect". This growth can cause compression of local tissues or organs, leading to many effects, such as blockage of ducts, reduced claret flow (ischaemia), tissue death (necrosis) and nerve pain or damage.[2] Some tumors too produce hormones that can atomic number 82 to life-threatening situations. Insulinomas tin can produce big amounts of insulin, causing hypoglycemia.[8] [9] Pituitary adenomas tin can crusade elevated levels of hormones such as growth hormone and insulin-like growth factor-one, which cause acromegaly; prolactin; ACTH and cortisol, which cause Cushings affliction; TSH, which causes hyperthyroidism; and FSH and LH.[10] Bowel intussusception can occur with various benign colonic tumors.[11] Cosmetic effects tin be caused by tumors, peculiarly those of the skin, possibly causing psychological or social discomfort for the person with the tumor.[12] Vascular tissue tumors tin drain, in some cases leading to anemia.[13]
Causes [edit]
PTEN hamartoma syndrome [edit]
PTEN hamartoma syndrome consists of 4 distinct hamartomatous disorders characterised by genetic mutations in the PTEN gene; Cowden syndrome, Bannayan-Riley-Ruvalcaba syndrome, Proteus syndrome and Proteus-like syndrome. Although they all take singled-out clinical features, the formation of hamartomas occurs in all four syndromes. PTEN is a tumor suppressor factor that is involved in cellular signalling. Absent-minded or dysfunctional PTEN protein allows cells to over-proliferate, causing hamartomas.[fourteen]
Other syndromes [edit]
Cowden syndrome is an autosomal dominant genetic disorder characterised by multiple benign hamartomas (trichilemmomas and mucocutaneous papillomatous papules) as well as a predisposition for cancers of multiple organs including the breast and thyroid.[15] [16] Bannayan-Riley-Ruvalcaba syndrome is a congenital disorder characterised by hamartomatous intestinal polyposis, macrocephaly, lipomatosis, hemangiomatosis and glans penis macules.[14] [17] Proteus syndrome is characterised by nevi, asymmetric overgrowth of various body parts, adipose tissue dysregulation, cystadenomas, adenomas, vascular malformation.[18] [19]

Familial adenomatous polyposis [edit]
Familial adenomatous polyposis (FAP) is a familial cancer syndrome acquired by mutations in the APC gene. In this disorder adenomatous polyps are present in the colon that volition progress into colon cancer unless removed.[20] The APC gene is a tumor suppressor; its protein production is involved in many cellular processes. Inactivation of the APC gene leads to the buildup of a protein called β-catenin, which activates ii transcription factors: T-cell factor (TCF) and lymphoid enhancer factor (LEF). These cause the upregulation of many genes involved in cell proliferation, differentiation, migration and apoptosis (programmed cell decease), causing the growth of beneficial tumors.[21]
Tuberous sclerosis circuitous [edit]
Tuberous sclerosis complex (TSC) is an autosomal dominant genetic disorder caused by mutations in the genesTSC1 and TSC2, which produce the proteins hamartin and tuberin, respectively. This disorder presents with many benign hamartomatous tumors including angiofibromas, renal angiomyolipomas, pulmonary lymphangiomyomatosis. Tuberin and hamartin inhibit the mTOR protein in normal cellular physiology and the inactivation of the TSC tumor suppressors causes an increase in mTOR action. This leads to the activation of genes and the product of proteins that increment prison cell growth.[22] [23] [24]
Von Hippel-Lindau illness [edit]
Von Hippel-Lindau disease is a dominantly-inherited cancer syndrome that significantly increases the risk of various tumors including benign hemangioblastomas and malignant pheochromocytomas, renal cell carcinomas, pancreatic endocrine tumors and endolymphatic sac tumors. It is acquired by genetic mutations in the Von Hippel–Lindau tumor suppressor gene. The VHL poly peptide (pVHL) is involved in cellular signalling in oxygen starved (hypoxic) cells. One role of pVHL is to cause the cellular deposition of some other protein, HIF1α. Dysfunctional pVHL leads to accumulation of HIF1α, which activates several genes responsible for the production of substances involved in prison cell growth and blood vessel production: VEGF, PDGFβ, TGFα and erythropoietin.[25]
Mechanism [edit]

Benign (L) vs Malignant tumor (R).
Benign vs cancerous [edit]
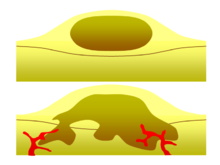
Diagram showing two epithelial tumors. The upper tumor is a beneficial tumor that is non-invasive. Benign tumors are usually round in shape and encapsulated by fibrous connective tissue. The lower picture depicts a malignant tumor. It is irregularly shaped, vascular, and it is invasive, crossing the basement membrane.
Ane of the most important factors in classifying a tumor as benign or malignant is its invasive potential. If a tumor lacks the ability to invade adjacent tissues or spread to distant sites past metastasizing so it is beneficial, whereas invasive or metastatic tumors are malignant.[two] For this reason, benign tumors are not classed as cancer.[iii] Benign tumors will grow in a contained area unremarkably encapsulated in a fibrous connective tissue capsule. The growth rates of beneficial and cancerous tumors also differ; benign tumors by and large grow more slowly than malignant tumors. Although benign tumors pose a lower health hazard than malignant tumors, they both tin can be life-threatening in certain situations. There are many full general characteristics which apply to either beneficial or cancerous tumors, just sometimes one blazon may show characteristics of the other. For instance, beneficial tumors are generally well differentiated and malignant tumors are often undifferentiated. Nevertheless, undifferentiated benign tumors and differentiated malignant tumors can occur.[26] [27] Although benign tumors generally grow slowly, cases of fast-growing benign tumors have too been documented.[28] Some malignant tumors are mostly non-metastatic such equally in the example of basal cell carcinoma.[iv] CT and chest radiography can be a useful diagnostic examination in visualizing a beneficial tumor and differentiating it from a cancerous tumor. The smaller the tumor on a radiograph the more likely information technology is to be benign as 80% of lung nodules less than two cm in bore are benign. Nigh benign nodules are smoothed radiopaque densities with articulate margins but these are not exclusive signs of benign tumors.[29]
Multistage carcinogenesis [edit]
Tumors are formed by carcinogenesis, a process in which cellular alterations pb to the formation of cancer. Multistage carcinogenesis involves the sequential genetic or epigenetic changes to a cell's DNA, where each pace produces a more than advanced tumor. It is often broken downwards into three stages; initiation, promotion and progression, and several mutations may occur at each stage. Initiation is where the first genetic mutation occurs in a jail cell. Promotion is the clonal expansion (repeated division) of this transformed cell into a visible tumor that is usually beneficial. Following promotion, progression may take place where more than genetic mutations are caused in a sub-population of tumor cells. Progression changes the benign tumor into a malignant tumor.[half-dozen] [xxx] A prominent and well studied example of this phenomenon is the tubular adenoma, a mutual type of colon polyp which is an important precursor to colon cancer. The cells in tubular adenomas, similar almost tumors that oft progress to cancer, show certain abnormalities of cell maturation and appearance collectively known as dysplasia. These cellular abnormalities are non seen in beneficial tumors that rarely or never plow malignant, but are seen in other pre-cancerous tissue abnormalities which exercise not class discrete masses, such every bit pre-cancerous lesions of the uterine cervix.
Diagnosis [edit]
Classification [edit]
| Cell origin | Cell blazon | Tumor |
|---|---|---|
| Endodermal | Biliary tree | Cholangioma |
| Colon | Colonic polyp | |
| Glandular | Adenoma | |
| Papilloma | ||
| Cystadenoma | ||
| Liver | Liver jail cell adenoma | |
| Placental | Hydatiform mole | |
| Renal | Renal tubular adenoma | |
| Squamous | Squamous cell papilloma | |
| Stomach | Gastric polyp | |
| Mesenchymal | Blood vessel | Hemangioma, Cardiac myxoma |
| Bone | Osteoma | |
| Cartilage | Chondroma | |
| Fat tissue | Lipoma | |
| Gristly tissue | Fibroma | |
| Lymphatic vessel | Lymphangioma | |
| Smooth musculus | Leiomyoma | |
| Striated muscle | Rhabdomyoma | |
| Ectodermal | Glia | Astrocytoma, Schwannoma |
| Melanocytes | Nevus | |
| Meninges | Meningioma | |
| Nerve cells | Ganglioneuroma | |
| Reference[31] | ||
Benign neoplasms are typically merely not always composed of cells which bear a strong resemblance to a normal jail cell blazon in their organ of origin. These tumors are named for the cell or tissue type from which they originate, followed by the suffix "-oma" (but non -carcinoma, -sarcoma, or -blastoma, which are mostly cancers). For example, a lipoma is a common beneficial tumor of fat cells (lipocytes), and a chondroma is a benign tumor of cartilage-forming cells (chondrocytes). Adenomas are beneficial tumors of gland-forming cells, and are unremarkably specified farther by their cell or organ of origin, as in hepatic adenoma (a benign tumor of hepatocytes, or liver cells). Teratomas contain many prison cell types such every bit peel, nervus, encephalon and thyroid, amid others, because they are derived from germ cells.[4] Hamartomas are a grouping of beneficial tumors that have relatively normal cellular differentiation but the architecture of the tissue is disorganised.[22] There are a few cancers with 'benign-sounding' names which have been retained for historical reasons, including melanoma (a cancer of pigmented skin cells, or melanocytes) and seminoma (a cancer of male reproductive cells).[32] Peel tags, song chord polyps and hyperplastic polyps of the colon are often referred to every bit beneficial but they are really overgrowths of normal tissue rather than neoplasms.[4]
Handling [edit]
Some benign tumors need no treatment; others may exist removed if they cause problems such as seizures, discomfort or corrective concerns. Surgery is usually the virtually constructive approach and is used to treat near benign tumors. In some example other treatments may be of use. Adenomas of the rectum may be treated with sclerotherapy, a handling in which chemicals are used to shrink blood vessels in guild to cutting off the blood supply.[13] Most benign tumors do not respond to chemotherapy or radiation therapy, although there are exceptions; beneficial intercranial tumors are sometimes treated with radiation therapy and chemotherapy under certain circumstances.[33] [34] Radiation tin besides be used to treat hemangiomas in the rectum.[xiii] Benign skin tumors are usually surgically resected simply other treatments such every bit cryotherapy, curettage, electrodesiccation, light amplification by stimulated emission of radiation therapy, dermabrasion, chemical peels and topical medication are used.[35] [36]
Proper noun [edit]
The give-and-take "beneficial" ways "favourable, kind, fortunate, salutary, propitious".[37] However, a "benign" tumour is not beneficial in the usual sense; the name merely specifies that information technology is not "malignant", i.e. cancerous. While benign tumours ordinarily do not pose a serious wellness gamble, they tin exist harmful or fatal.[38]
References [edit]
- ^ "What Is Cancer?". National Cancer Institute. 2007-09-17. Retrieved 2017-11-26 .
 This article incorporates text from this source, which is in the public domain .
This article incorporates text from this source, which is in the public domain . - ^ a b c d Wilson KA, Waugh A, Chambers G, Grant A, Ross J (2006). Ross and Wilson anatomy and physiology in health and illness. Edinburgh: Churchill Livingstone. pp. 53–54. ISBN0-443-10101-ix.
- ^ a b Nunn LS, Silverstein A, Silverstein VB (2006). Cancer . Brookfield, Conn: Twenty-First Century Books. pp. 11–12. ISBN0-7613-2833-5.
- ^ a b c d Strayer DL, Rubin R, Rubin E (2008). Rubin'south pathology: clinicopathologic foundations of medicine. Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins. pp. 138–139. ISBN978-0-7817-9516-half-dozen.
- ^ Ober WB, Martini F (2006). Fundamentals of anatomy & physiology. San Francisco: Pearson Benjamin Cummings. ISBN0-321-31198-1.
- ^ a b Clark WH (Oct 1991). "Tumour progression and the nature of cancer". British Journal of Cancer. 64 (4): 631–644. doi:10.1038/bjc.1991.375. PMC1977704. PMID 1911211.
- ^ Reece J, Campbell N, Urry Fifty (2005). Biology. San Francisco: Pearson Benjamin Cummings. p. 232. ISBN0-321-27045-two.
- ^ Marks 5, Teale JD (June 1991). "Tumours producing hypoglycaemia". Diabetes/Metabolism Reviews. vii (2): 79–91. doi:ten.1002/dmr.5610070202. PMID 1665409.
- ^ Grant CS (Oct 2005). "Insulinoma". All-time Do & Research. Clinical Gastroenterology. 19 (5): 783–798. doi:10.1016/j.bpg.2005.05.008. PMID 16253900.
- ^ Eng C, DeLellis RA, Lloyd RV, Heitz PU (2004). Pathology and genetics of tumours of endocrine organs. Lyon: IARC Printing. ISBN92-832-2416-vii.
- ^ Gill SS, Heuman DM, Mihas AA (October 2001). "Small intestinal neoplasms". Periodical of Clinical Gastroenterology. 33 (4): 267–282. doi:x.1097/00004836-200110000-00004. PMID 11588539.
- ^ Tromberg J, Bauer B, Benvenuto-Andrade C, Marghoob AA (2005). "Congenital melanocytic nevi needing treatment". Dermatologic Therapy. 18 (2): 136–150. doi:10.1111/j.1529-8019.2005.05012.x. PMID 15953143. S2CID 20915929.
- ^ a b c Zuber Thousand, Harder F (2001). Benign tumors of the colon and rectum. Munich: Zuckschwerdt: Surgical Handling: Evidence-Based and Problem-Oriented.
- ^ a b Hobert JA, Eng C (Oct 2009). "PTEN hamartoma tumor syndrome: an overview". Genetics in Medicine. 11 (10): 687–694. doi:10.1097/GIM.0b013e3181ac9aea. PMID 19668082.
- ^ Pilarski R, Eng C (May 2004). "Will the existent Cowden syndrome please stand up (again)? Expanding mutational and clinical spectra of the PTEN hamartoma tumour syndrome". Journal of Medical Genetics. 41 (five): 323–326. doi:10.1136/jmg.2004.018036. PMC1735782. PMID 15121767.
- ^ Eng C (Nov 2000). "Will the real Cowden syndrome please stand up: revised diagnostic criteria". Journal of Medical Genetics. 37 (xi): 828–830. doi:10.1136/jmg.37.11.828. PMC1734465. PMID 11073535.
- ^ Eng C (September 2003). "PTEN: one factor, many syndromes". Human Mutation. 22 (3): 183–198. doi:x.1002/humu.10257. PMID 12938083. S2CID 13417857.
- ^ Blumenthal GM, Dennis PA (November 2008). "PTEN hamartoma tumor syndromes". European Journal of Man Genetics. 16 (11): 1289–1300. doi:10.1038/ejhg.2008.162. PMC6939673. PMID 18781191.
- ^ Cohen MM (August 2005). "Proteus syndrome: an update". American Journal of Medical Genetics. Part C, Seminars in Medical Genetics. 137C (1): 38–52. doi:10.1002/ajmg.c.30063. PMID 16010681. S2CID 31873101.
- ^ Galiatsatos P, Foulkes WD (February 2006). "Familial adenomatous polyposis". The American Periodical of Gastroenterology. 101 (2): 385–398. doi:10.1111/j.1572-0241.2006.00375.x. PMID 16454848.
- ^ Aoki K, Taketo MM (October 2007). "Adenomatous polyposis coli (APC): a multi-functional tumor suppressor gene". Periodical of Prison cell Science. 120 (Pt xix): 3327–3335. doi:10.1242/jcs.03485. PMID 17881494. S2CID 8743.
- ^ a b Inoki G, Corradetti MN, Guan KL (January 2005). "Dysregulation of the TSC-mTOR pathway in human disease". Nature Genetics. 37 (ane): 19–24. doi:ten.1038/ng1494. PMID 15624019. S2CID 205344131.
- ^ Crino PB, Nathanson KL, Henske EP (September 2006). "The tuberous sclerosis complex". The New England Periodical of Medicine. 355 (13): 1345–1356. doi:10.1056/NEJMra055323. PMID 17005952. S2CID 3579356.
- ^ Kwiatkowski DJ (January 2003). "Tuberous sclerosis: from tubers to mTOR". Annals of Human being Genetics. 67 (Pt i): 87–96. doi:10.1046/j.1469-1809.2003.00012.x. PMID 12556239. S2CID 41992893.
- ^ Maher ER (December 2004). "Von Hippel-Lindau illness". Current Molecular Medicine. four (8): 833–842. doi:10.2174/1566524043359827. PMID 15579030.
- ^ Skorić T, Korsić M, Zarković K, Plavsić V, Besenski Due north, Breskovac 50, et al. (June 1999). "Clinical and morphological features of undifferentiated monomorphous GH/TSH-secreting pituitary adenoma". European Periodical of Endocrinology. 140 (6): 528–537. doi:ten.1530/eje.0.1400528. PMID 10366409.
- ^ Song HJ, Xue YL, Qiu ZL, Luo QY (2012). "Uncommon metastases from differentiated thyroid carcinoma". Hellenic Journal of Nuclear Medicine. fifteen (3): 233–240. PMID 23106056.
- ^ Sagel SS, Ablow RC (Nov 1968). "Hamartoma: on occasion a rapidly growing tumor of the lung". Radiology. 91 (5): 971–972. doi:10.1148/91.5.971. PMID 5681331.
- ^ Erasmus JJ, Connolly JE, McAdams HP, Roggli VL (2000). "Lonely pulmonary nodules: Part I. Morphologic evaluation for differentiation of beneficial and malignant lesions". Radiographics. 20 (1): 43–58. doi:10.1148/radiographics.xx.1.g00ja0343. PMID 10682770.
- ^ Barrett JC (April 1993). "Mechanisms of multistep carcinogenesis and carcinogen risk assessment". Environmental Health Perspectives. 100: 9–20. doi:10.1289/ehp.931009. PMC1519586. PMID 8354184.
- ^ Wujcik D, Yarbro CH, Gobel BH (2011). Cancer nursing: principles and practice. Boston: Jones and Bartlett Publishers. ISBN978-0-7637-6357-two.
- ^ Cotran R, Kumar Five, Collins T (1999). Robbins Pathologic Basis of Disease (6th ed.). W.B. Saunders. ISBN0-7216-7335-Ten.
- ^ Brada Thou (Feb 2013). "Radiotherapy for beneficial encephalon tumours coming of age; instance of vestibular schwannoma". Radiotherapy and Oncology. 106 (2): 157–160. doi:ten.1016/j.radonc.2013.01.009. PMID 23462704.
- ^ Sioka C, Kyritsis AP (March 2009). "Chemotherapy, hormonal therapy, and immunotherapy for recurrent meningiomas". Periodical of Neuro-Oncology. 92 (ane): 1–six. doi:10.1007/s11060-008-9734-y. PMID 19023520. S2CID 28106960.
- ^ Luba MC, Bangs SA, Mohler AM, Stulberg DL (February 2003). "Mutual benign peel tumors". American Family unit Physician. 67 (4): 729–738. PMID 12613727.
- ^ Marghoob AA, Borrego JP, Halpern AC (December 2007). "Built melanocytic nevi: treatment modalities and management options". Seminars in Cutaneous Medicine and Surgery. 26 (4): 231–240. doi:10.1016/j.sder.2008.03.007. PMID 18395671.
- ^ "beneficial". Oxford English language Lexicon (Online ed.). Oxford University Press. (Subscription or participating institution membership required.)
- ^ Rao AK (Feb 2021). "Overview of Heart Tumors - Treatment of noncancerous (benign) heart tumors". MSD Transmission Consumer Version.
Children with this type of [inoperable, benign] tumor usually die of an abnormal center rhythm at an early on age.
External links [edit]
Source: https://en.wikipedia.org/wiki/Benign_tumor
0 Response to "Are Benign Tumors Are Likely to Spread to Different Parts of the Family?"
إرسال تعليق